Written & Art by Farah Yasmin binti Firdaus Suffian
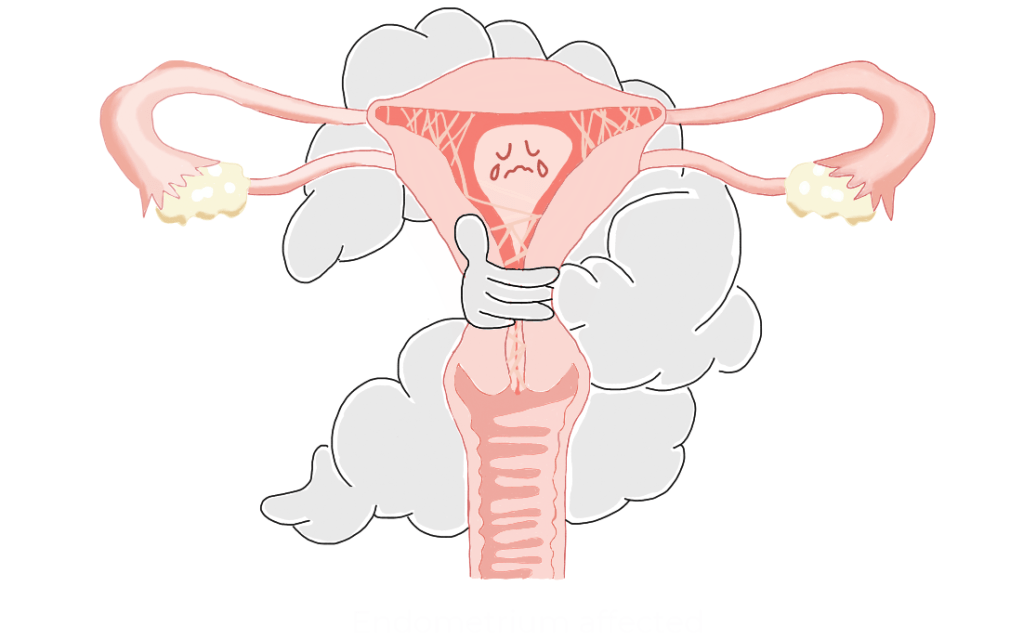
Scar tissue doesn’t just heal–it can strangle. Asherman’s syndrome, also known as intrauterine adhesions or synechiae, occurs when scar tissue forms inside the uterus and/or cervix, affecting up to 1.5% of infertile women and a staggering 46% after repeated hysteroscopic resections. While some patients exhibit normal ovulation and menstrual cycles (if adhesions are partial), others suffer hypomenorrhea, amenorrhea, or crippling dysmenorrhea. Recurrent miscarriage and infertility are warning signs; severe cases may cause uterine blockage and retrograde menstruation, where blood flows backwards into the fallopian tubes instead of exiting the body.
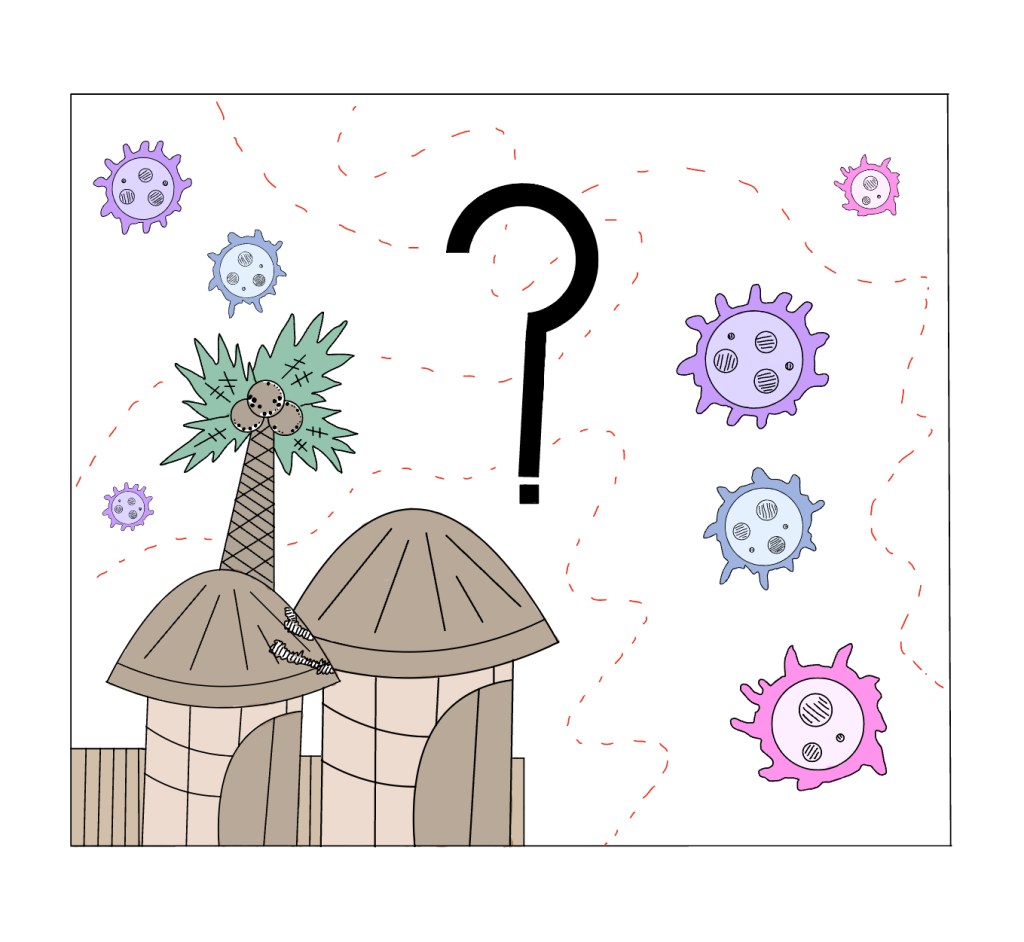
This scarring typically occurs after uterine trauma, most commonly following postpartum or post-miscarriage dilation and curettage (D&C). It may also develop after fibroid removal surgeries or endometrial ablation procedures used to control excessive bleeding. In developing regions, genital tuberculosis or schistosomiasis infections can similarly trigger these dangerous adhesions.
Diagnosing Asherman’s requires specialised approaches when standard hormone tests show normal function yet menstruation remains absent. While ultrasounds hint at adhesions, saline sonography or hysterosalpingography provide better detection (though sensitivity remains just 75%). The gold standard is hysteroscopy, which both visualises and treats adhesions simultaneously; MRI is reserved for total uterine obliteration. Treatment demands precision: hysteroscopic adhesiolysis (using microscissors to minimize new scarring), paired with adjuvant therapies like estrogen supplementation to promote endometrial growth, temporary intrauterine devices or balloons to prevent re-adhesion, and emerging options such as stem cell therapy and anti-adhesion gels. Despite treatment, the condition frequently recurs, necessitating repeated procedures and close postoperative monitoring.
Even with treatment, women face recurrent pregnancy losses as adhesions frequently return after surgical removal (adhesiolysis). The scarring also creates unique cancer risks. While endometrial cancer may be less common, crucial warning signs like abnormal bleeding can be masked by the adhesions. Regular ultrasound monitoring becomes essential to detect any dangerous changes. Most cruelly, a healthy uterine lining is vital for pregnancy. However, these scars silently sabotage implantation, increase miscarriage risks, and cause late-term complications, all while leaving no outward clues.
Asherman’s syndrome is a stealthy reproductive thief–its scars invisible, its consequences devastating. Despite medical advances, its persistence and emotional toll demand greater awareness, refined treatment, and compassionate care for women battling this invisible condition. The scars may be internal, but the struggle is profoundly real.
Works cited:
- Smikle C., Yarrarapu, S., Khetarpal S. Asherman Syndrome. StatPearls [Internet]. Updated 2023 July 24 [cited 2025 March 28]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448088/#:~:text=Asherman%20syndrome%20(intrauterine%20adhesions%20or,being%20a%20less%20common%20cause
- National Organisation for Rare Disorders. Asherman’s Syndrome. National Organisation for Rare Disorders (NORD) [Internet]. Updated 2021 March 15. Available from: https://rarediseases.org/rare-diseases/ashermans-syndrome/
- Inception Fertility. Intrauterine Adhesions, Asherman’s Syndrome – Scar Tissue in Uterine Cavity. Advanced Fertility [Internet]. 2020 Sep 17. Accessed 2025 Mar 28. Available from: https://www.advancedfertility.com/blog/intrauterine-adhesions-ashermans-syndrome-scar-tissue-in-uterine-cavity

Leave a comment