Written by Aashna Gupta | Art by MollyAnn Caulfield
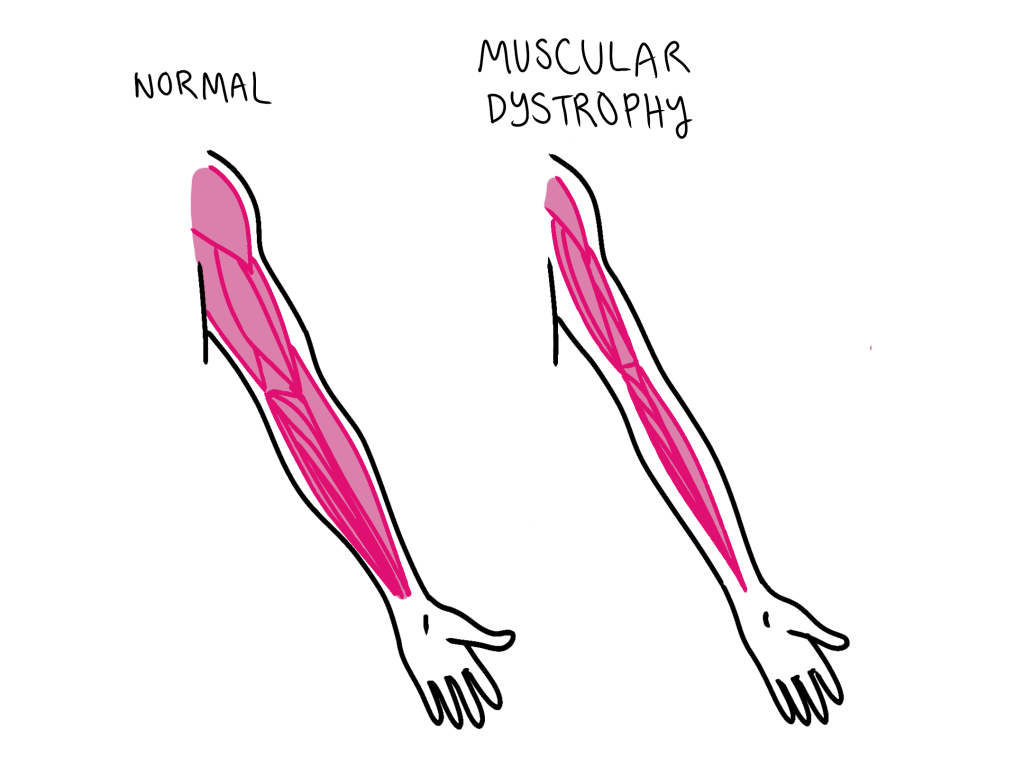
Duchenne Muscular Dystrophy (DMD), one of the most severe and common forms of muscular dystrophy, is a sex-linked disorder, affecting approximately 1 in every 3,500 to 5,000 male births worldwide. DMD is a genetic disorder that causes progressive muscle degeneration and weakness due to the absence of dystrophin, which is a protein essential for maintaining healthy muscle function. Though it primarily affects males, it can also be carried by females, who may experience milder symptoms.
DMD typically begins to show signs in early childhood, often between the ages of 2 and 5. Children with DMD may experience difficulty walking, running, or climbing stairs. As the disease progresses, muscle weakness spreads from the pelvis and legs to the arms, neck, and other areas. By the teenage years, many individuals with DMD require a wheelchair for mobility. The heart and respiratory muscles are also impacted over time, leading to serious complications.
What makes Duchenne Muscular Dystrophy particularly devastating is its progressive nature. Muscle tissue is gradually replaced by fat and connective tissue, leading to a continuous loss of strength and function. In addition to physical symptoms, individuals with DMD may also face learning difficulties or cognitive challenges, although these vary from person to person.
Duchenne Muscular Dystrophy is caused by mutations in the DMD gene located on the X chromosome. Because males have only one X chromosome, a mutation in this gene usually results in the disease. Females with one mutated copy are typically carriers and might not show severe symptoms. Unlike conditions linked to environmental exposure, DMD is entirely genetic and is passed down through families or occurs as a spontaneous mutation.
Currently, there is no cure for Duchenne Muscular Dystrophy. However, there are treatments that can help manage symptoms and improve quality of life. Corticosteroids, for example, can slow muscle degeneration. Physical therapy, respiratory care, and cardiac monitoring also play essential roles in managing the disease. New therapies, including gene-based treatments and exon-skipping drugs, offer hope and are actively being explored through ongoing research.
As with many rare diseases, increasing public awareness and funding for research are essential. Early diagnosis, supportive care, and advancements in treatment can make a significant difference in the lives of those affected by DMD. Through education, advocacy, and continued scientific innovation, we move closer to understanding and eventually overcoming Duchenne Muscular Dystrophy.
Citations:
Muscular Dystrophy Association. “Duchenne Muscular Dystrophy.” MDA, 2024, www.mda.org/disease/duchenne-muscular-dystrophy.
Centers for Disease Control and Prevention. “Duchenne and Becker Muscular Dystrophy.” CDC, 2023, www.cdc.gov/ncbddd/musculardystrophy/facts.html.
Genetics Home Reference. “Duchenne and Becker Muscular Dystrophy.” MedlinePlus Genetics, U.S. National Library of Medicine, 2024, http://www.medlineplus.gov/genetics/condition/duchenne-and-becker-muscular-dystrophy.

Leave a comment